The Comprehensive Guide to Risks of Partial Hysterectomy and Women's Health

In the realm of women's health, surgical interventions such as partial hysterectomy are common procedures performed to address various gynecological conditions. While these surgeries can offer dramatic improvements in quality of life, they also come with potential risks that both patients and healthcare providers must consider thoroughly. Understanding the risks of partial hysterectomy is crucial for making informed decisions and ensuring optimal health outcomes.
Understanding Partial Hysterectomy: Definition and Indications
Partial hysterectomy, also known as subtotal hysterectomy, involves the removal of the uterus while leaving the cervix intact. This surgical approach is typically indicated for conditions such as fibroids, endometriosis, abnormal uterine bleeding, and precancerous lesions. It is often preferred for its shorter recovery time and preservation of cervical function, which can benefit certain women.
Why Women Might Consider a Partial Hysterectomy
- Relief from chronic pain and bleeding: Conditions like fibroids or adenomyosis causing heavy bleeding or pain.
- Prevention of disease progression: Addressing precancerous changes or preventing future malignancies.
- Minimally invasive options: Partial hysterectomy can sometimes be performed laparoscopically, reducing recovery time.
- Desire to retain cervical function: For some women, preserving the cervix helps maintain sexual function and pelvic stability.
The Risks of Partial Hysterectomy: An In-Depth Analysis
While many women undergo partial hysterectomy successfully, it is vital to be aware of the potential complications and risks. These risks can vary depending on individual health status, age, surgical technique, and the skill of the surgical team. Here, we explore these risks of partial hysterectomy in detail.
Immediate Surgical Risks
- Bleeding and Hemorrhage: Excessive intraoperative bleeding may require blood transfusions or additional interventions.
- Infection: Like all surgeries, there is a risk of infection at the surgical site or within the pelvic cavity.
- Damage to Surrounding Organs: The bladder, ureters, or intestines can inadvertently be injured during surgery, leading to complex medical issues.
- Anesthesia Complications: Reactions to anesthesia, including respiratory issues or cardiovascular problems.
Long-Term and Postoperative Risks
- Changes in Pelvic Support and Posture: Removal of the uterus can weaken pelvic support structures, potentially leading to prolapse complications over time.
- Altered Sexual Function: While many women report preserved sexual satisfaction, some may experience changes linked to nerve disruption or psychological factors.
- Psychological Impacts: Feelings of loss or changes in body image can affect mental health, especially if the hysterectomy was performed for cancer or other traumatic reasons.
- Risk of Cervical-Related Complications: Since the cervix is preserved, conditions like cervical stenosis or continued cervical pathology may still pose problems.
- Potential for Future Surgical Interventions: Possibility of additional surgeries if complications such as pelvic organ prolapse arise.
Specific Risks of Partial Hysterectomy Compared to Total Hysterectomy
Understanding the distinctions in risks between partial and total hysterectomy is critical. While partial hysterectomy preserves the cervix, it also maintains certain risk factors associated with the remaining cervical tissue. These include:
- Cervical Cancer Risks: The preserved cervix requires continued screening through Pap smears and HPV testing.
- Persistent or New Cervical Pathology: Conditions like cervical dysplasia or infections can still develop post-surgery.
- Residual Symptoms: Some women may continue to experience symptoms related to the cervix or underlying pathology.
Managing and Mitigating Risks: The Role of Expert Gynecologists at drseckin.com
At drseckin.com, a team of experienced obstetricians and gynecologists is dedicated to providing personalized, comprehensive care that minimizes surgical risks. They implement best practices including:
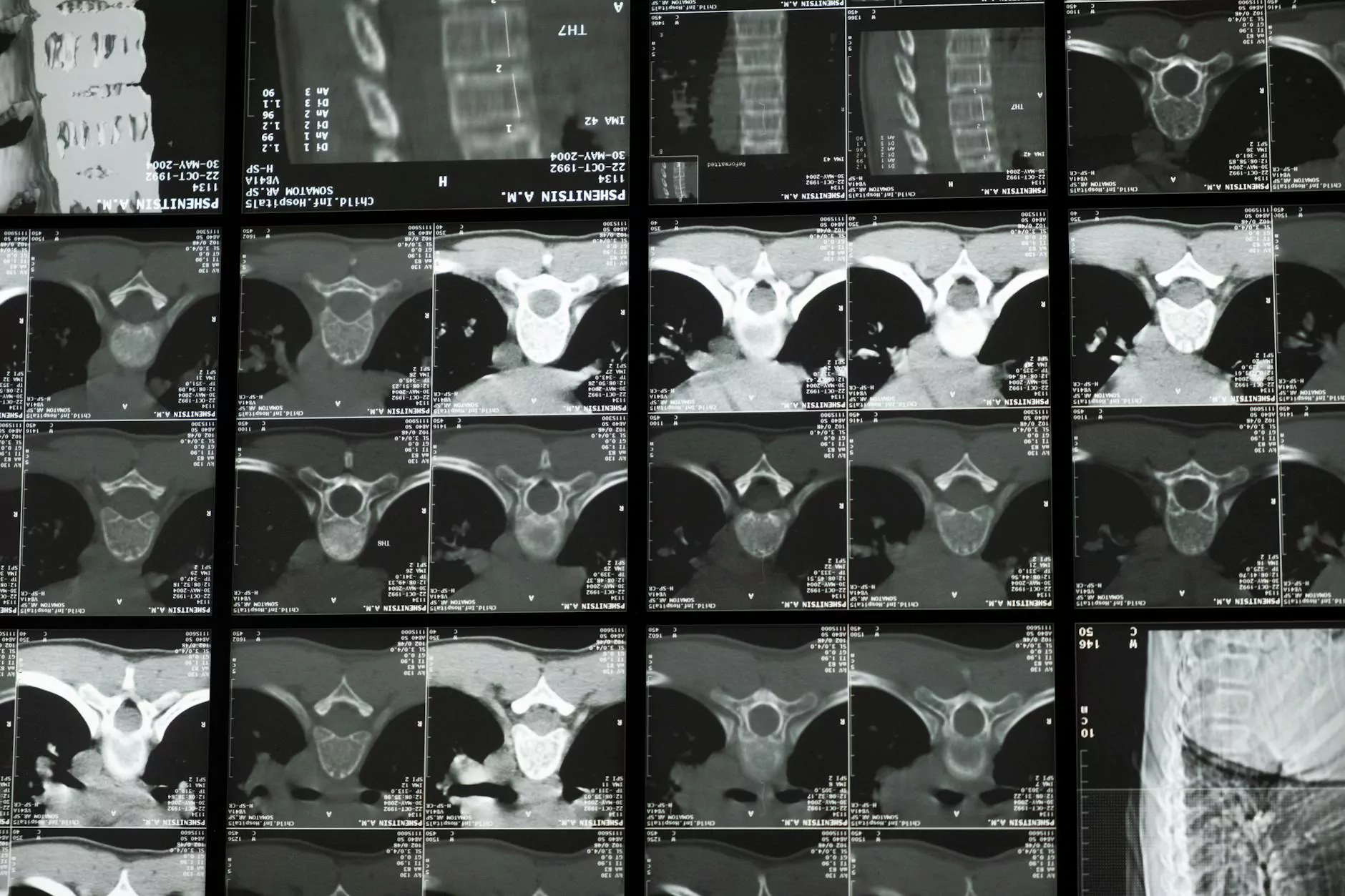
- Preoperative Evaluation: Thorough assessment of individual health, imaging, and pathology to ensure suitability for surgery.
- Advanced Surgical Techniques: Utilizing minimally invasive approaches such as laparoscopic or robot-assisted surgeries to reduce complications.
- Intraoperative Precision: Careful dissection and preservation of surrounding structures to prevent injury.
- Postoperative Monitoring: Close follow-up to detect and manage any early or late-occurring complications.
- Patient Education: Providing detailed information on postoperative care, warning signs, and long-term health monitoring.
Long-Term Considerations and Follow-Up Care
Maintaining long-term health after a partial hysterectomy involves vigilant follow-up and lifestyle adjustments:
- Continued Cervical Screening: Regular Pap smears to detect any precancerous changes.
- Pelvic Floor Exercises: Strengthening pelvic support muscles can prevent prolapse and improve quality of life.
- Healthy Lifestyle: Maintaining a balanced diet, regular exercise, and avoiding smoking can reduce additional health risks.
- Monitoring for Symptoms: Reporting any new pelvic pain, unusual bleeding, or urinary issues promptly.
The Future of Women's Gynecological Surgery
Advancements in medical technology and surgical techniques continue to improve outcomes and reduce risks of partial hysterectomy. Innovations include robotic-assisted surgeries, better imaging guidance, and personalized surgical planning based on genetic and hormonal profiles. Moreover, comprehensive patient education and multidisciplinary care contribute significantly to safer procedures and enhanced recovery.
Choosing the Right Healthcare Partner for Your Gynecological Needs
Seamless, safe, and effective management of gynecological conditions begins with selecting an experienced and compassionate healthcare team. drseckin.com provides expert care, emphasizing:
- Patient-centered approach: Tailoring treatment plans to individual needs, preferences, and health status.
- Transparency and Communication: Ensuring patients are fully informed about procedures, advantages, and potential risks.
- Comprehensive Support: From diagnosis through recovery, offering guidance and reassurance at every step.
Conclusion: Informed Decisions Lead to Better Outcomes
Understanding the risks of partial hysterectomy empowers women to make informed, confident choices regarding their reproductive and overall health. While the procedure offers many benefits, awareness of possible complications ensures preparedness and proactive management. Consulting with experienced obstetricians and gynecologists at reputable centers like drseckin.com guarantees state-of-the-art care, personalized attention, and optimal health outcomes for women seeking relief from gynecological issues.
Remember, the journey toward health is a partnership — education, expert guidance, and vigilance are your best tools for a safe and positive surgical experience.